Brussels
Airlines dropped me in the middle of the rain.
Airport
control was chaotic as could be expected but I succeeded to find a successful
track to my luggage. My suitcase had already been taken from the belt, but theft
was prevented by checking the tag at the exit.
My
daughter had told me the story of two doctors who took a common taxi at an African
airport and they never showed up again.
Being
welcomed by my name on a sign hold up by a driver and accompanying car, felt as
a first guarantee for safety within a country that had suffered civil war and Ebola
for decades.
As many West African countries, Liberia had been a transit point in slavery transport.
In the beginning of the 19th century, relieved black American slaves came back to Liberia to establish firstly an American country and then an independent state oriented to American structures and values.
In the beginning of the 19th century, relieved black American slaves came back to Liberia to establish firstly an American country and then an independent state oriented to American structures and values.
During the last two centuries, Liberia
has always been exploited and abused by other countries through poorly
negotiated contracts
because of their mining products (rubber and others).
It was only in the sixties that native Liberians
obtained the right to vote and in the nineties and in the beginning of the 3rd
millennium a
terrifying civil war occurred over the country.
One of the former presidents
Samuel Doe was
killed by Prince Johnson in a cruel way and the government of Charles Taylor, lasting until 2006, was nothing less than an
authoritarian military state.
It took until the presidency
of Mrs. Ellen Johnson,
as the first female president in Africa, in 2006, that a peaceful transition to democracy occurred.
She came from the World Bank and established at
least on the
political side
a more stable
government but
economic development
was almost
completely destroyed
by the Ebola crisis in 2014.
Recently her party lost the elections
and since one year a famous formal
football player,
George Weah, has taken the highest position in the country.
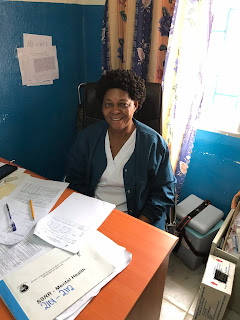
I was welcomed by Florence
-I thought Nightingale- but she died a long time ago, or Griffith- but her
nails where short cut- and it took me a few rehearsals to remember that her
last name was Yahnquee Kiatamba.
Beside Zoe Doe, she was
part of the NCD team headed by Dr Fred Amegashie, a distinct cell within the
Ministery of Health responsible for the management of Non Communicable Disease
as diabetes, hypertension, COPD and cancer.
At the occasion of the
Health Policy program in the Tropical Institute of Antwerp, I met Vera Mussah, head
of the PBF unit of the Liberian Ministery, and she created the opportunity for
a mission of our team focused on cancer policy in Liberia.During the following interviews, I would learn that the last name revealed whether people were from an Afro-American background (10%) or a native Liberian background (90%).
At this moment -writing
the story- the guardian who had started to shout to all the drivers who tried
to find a spot at the hotel parking, came to me a little hesitating to request
whether I could move a little bit to the left.
I presumed he had
waited for more than half an hour to dare chasing me away and I rewarded his
courage by moving friendly to the place he designed me.
Anyway, short pants and
a white skin still makes the difference.
Florence guided me to the
suburbs of the ministerial kingdom with the request whether I could have a
short talk with Mrs. Jallah,
She didn’t seem to have
the right position or credentials to pass the bureaucracy and while going back
to her office she suddenly was called back that the minister was available to
see us.
All the barriers fell down
until we arrived at the door of the minister’s office :" strictly forbidden to
take electronic devices within the office.”
A few urgent matters preceded
us in the waiting queue until we were welcomed by Mrs.
At the end of my 2-days
interview itinerary, I would never had postulated that the ambition of the project
was to establish Liberia as an example for cancer policy and her slightly
cynical look at the occasion of my remark, taught me that my cheap buy-in wasn’t
really appreciated.
As I would learn in the
following interviews, my introduction about my professional background was
politely accepted but not more than a step over to the presentation of my dialogue
partner’s history, beliefs, ideas and intentions.
The minister wanted to
establish five or six ambulatory cancer centres in the country for prevention,
counselling, screening, early diagnosis and chemotherapy treatment. She was in
favour of independent small cancer centres as a kernel of expertise from where
people could be referred to hospitals if necessary for example in case of
surgery.
She referred me to Dr. Ann
Marie Beddoe, an American gynaecologist who was doing some developing work in
the JFK University Hospital for many years.
Mrs Jallah reassured access
of me to her the same day by giving her an instant call.
The minister-assistant
of prevention, Joyce Sherman, seemed to have no intense connection with the
cancer policy.
She was more specific
about programs on diabetic education and the delivery of HPV-vaccines to 14/16
years old girls.
She had worked for the
WHO, USAID and since twelve years for the Liberian government.
She had a bachelor in
nursing with an attention for public and child health.
She emphasised that the
initiatives concerning cancer were fragmented and the aim was to analyse what
was already there and then connecting the dots.
“There is no lack of
evidence and nice policy documents”, she emphasised : “but it all blocks at the
level of implementation.”
90% of the health
budget of Liberia was spent on the pay of employees and administration. So only
10% was available for service delivery.
We had to realise that
all improvement in infrastructure, education and quality had to be funded by third
parties.
At this moment at JFK,
a 5-million-dollar medical image center with MRI and CT was built with American
money.
Driving from the hotel
to the ministry, I remembered the construction of a huge new building for
government agencies, sponsored by the Chinese and later the Japanese would
welcome us in the JFK building for maternal care: the international competition
for conquering Africa by development aid….
One hour later, again
we had to pass the initial barrier of bureaucracy to meet Dr. Kaieh, the
chief medical officer of the Ministry of Health.
Although it seemed to
me that Florence had made appointments with all these responsible people,
nevertheless every time we were welcomed as an unexpected guest.
It seemed that 20
minutes of humble waiting was building up a minimum level of confidence to be accepted
for a visit.
Entering
the office of Dr. Kaieh was like entering a world of rewards an certificates of
high standard education with a kind of military flavour due to his tight suit.
He
tolerated a short introduction of myself and then he referred me to a picture
on the wall with a woman and a young boy lying on a bed.
“That’s
why I’m here”, he started his story : “My mother was blind at one eye and I was
mocked for that at school. She had had bacterial conjunctivitis.
Although
we were poor and there was no perspective for university, I promised my mother
I would become a doctor and travel in Liberia from city to city to deliver to
the people convenient care.
When
I had finished high school, I had no opportunity to obtain a master’s degree or
to become a medical doctor as I had dreamed.
So,
I started to do voluntary work in hospitals such as cleaning, until I was
noticed by a surgeon, dr Stevenson, who was surprised I was spying his clinical
work in the operation theatre. He offered me to pay for obtaining a university
degree but unfortunately, he died after two years.
But
I got a scholarship to have a medical education in the United States where I
obtained my medical degree from 1988 to 1995.
In
the meantime, my mother had died during the civil war in 1994.
After
graduation, I came back to Liberia and worked at JFK, and from 1998 to 2001 I
was medical director at the Ganta Hospital.
Within
the political tense and dangerous situation, I got almost killed and I left the
country for the United States in 2001.
I
worked in the Sacred Hospital of Chicago and after a while I completed a master
in health care administration.
From
2004 to the end of 2010, I was the public health director in North Carolina.
I
asked my father to move out from Liberia and to join me in the United States
but he refused.
I
was applying for another job in New York as coincidently I focused on the
picture of me and my mother lying on the bed and I started crying.
I
realised I had not fulfilled my promise.
In
search of a new house in New York, I got a call from the president of Liberia,
Ellen Johnson, who wanted me to give a speech at the inauguration of a hospital
constructed by the Chinese in Tapeta, the 26th July 2010.
It
was a brand-new hospital built next to an old one once constructed by the
Taiwanese but partly destroyed during the war.
At
the occasion of this inauguration, I met the Chinese ambassador and aligned
with president Johnson, they both convinced me to take the lead of this
hospital.
I
could not resist to keep my promise to my mother and to come back to Liberia,
although I lost my wife by this.
Due
to my expertise in prevention of biological war, I became the medical
responsible for Ebola policy and when the epidemic was over, I arrived at this
post of chief medical officer."
He
didn’t seem to appreciate I shortly interrupted his story as his loyalty to his
mother and the fulfilling of his promise had become the mantra of his life
which he wanted to share as a kind of universal mission.
“What
do you want to achieve in the following years, what’s your dream?” I tried to
connect his impressive story to a new challenge for the future
“If
you really want to change something in the system, it all starts with leadership
and management”, he answered : “My dream is to establish a high end health care
management education as a leverage for a better quality of care in Liberia.”
“Maybe
we can be partners.” I aligned to his mission.
Dr.
Cooper was the Assistant Minister for Curative Care.
She
explained that except of the public sector (about 75%) there were a lot of
faith-based hospitals and also private for profit institutes in Liberia.
Concerning
new initiatives, she referred to the medical imaging centre that was built now in
JFK, the plans for radiotherapy, the actual chemotherapy unit in Hope for Women
and the nearby establishment of a state of the art unit for breast cancer and
cervix cancer in JFK in cooperation with dr. Ann Marie Beddoe.
For
specialised training for doctors she referred to the programs of of the
Liberian College of Physicians and Surgeons and she admitted that for most
highly specialised medical education ,doctors had to be send abroad.
Her
lack of Liberian accent and the light brown color of her skin, revealed that
she was an American.
Ann
Marie Bedoe had had a professional career as a gynaecologist, but she had
limited her clinical activity, that means she stopped doing surgery but was
still involved in clinical oncology especially for breast and cervix cancer.
She
had a special interest for global and woman’s health.
She
started to do some voluntary work in the JFK hospital about 10 years ago and
recently she was also involved in a project on building health work force
funded by the World Bank.
Her
support in enhancing quality in breast and cervix cancer was not funded by this
project but by her private donation fund.
She
came to Libera about every 2 months.
During
the last years she took the initiative to train a pharmacist and a nurse in the
Mount Sinai hospital in New York, in order to prepare and administer
chemotherapy. For diagnosis they worked with FNA, or Fine Needle Aspirations.
At
the moment, the unit for gynaecology and maternity had the disposition of an
Ugandan pathologist and a second one in the country was linked to the hospital
in Tapeta while three other pathologists were in training in Ghana.
In
the future they considered tele-consulting for complex case.
Laminar
airflow furniture for more or less safe preparation of anti-cancer drugs was
available.
The
budget for cytostatic drugs was still a problem.
For
screening she had proposed a method of visual inspection with acetic acid
smears. Screening of APV was ongoing but palliative care was an issue. It was
her conviction that first a palliative care unit within the university hospital
should be set up with education of nurses and social workers and from that
point as a leverage for home care.
In
her opinion, conditions were acceptable to start up with the chemotherapy unit
in September.
At
the occasion of a short visit at the chemotherapy unit in the private facility “Hope
for Women”, we met one patient who couldn’t attend the day before and she was
alone because treatment was only 3 days a week.
I
wondered, based on my experience as hospital manager, how they could provide
three nurses for one patient and since the staff was available, why not
treating more patients?
The
chemo was prescribed in the paper medical file of the patients and apparently
nurses mixed the anti-cancer drugs without special precautions.
Dr.
Ann Marie Bedoe tried to hide some little skepticism concerning the quality and
safety of this ambulatory unit.
She
admitted that she had held the pen in the extensive cancer policy letter that
was prepared and approved by the cancer committee.
Initially
focus would be put on breast and cervix cancer.
Having read it thoroughly, it elicited in me a great respect for the clinical knowledge and strategic vision with “smart” goals in setting up this policy, although I felt quite a substantial gap between the medical / public health language and concepts and the extent to with the NCD-committee would be able to materialise the requirements and implement the program.
Having read it thoroughly, it elicited in me a great respect for the clinical knowledge and strategic vision with “smart” goals in setting up this policy, although I felt quite a substantial gap between the medical / public health language and concepts and the extent to with the NCD-committee would be able to materialise the requirements and implement the program.
Next day we were not welcomed by Adolfos Kenta, the community
health department director van Montserrado County.
After
a short talk with one of her deputies, a sudden intense teleconferencing
indicated that the big boss was considering to join us.
“Mr.
Deputy” was banned to the next table and we started our explorative meeting on
NCDs, especially cancer.
I
stucked a while with the administrative reporting system as we were shown that
all relevant administrative and medical information had to be filled in in a
prestructured form by the treating doctor or nurse.
Information
from these individual files was aggregated in a huge book as a kind of super excel
on paper, which was the base for - still written on paper - statistics on
number of deliveries and others.
This
form was sent to the county where three people did the input in the DHIS2-system,
the national medical / administrative database as a kind of datawarehouse that
was aimed to guide health care policy on the county level and the national
level. Now structured data were gathered on cancer so that screening or early
diagnoses mostly depended on the knowledge and attention of the care provider.
Dr.
Kenta was not aware of any training for cancer prevention screening, diagnosis
of treatment within the last year.
Nevertheless,
she pointed out that it was necessary.
Slightly
opposing her quite passive attitude, I wondered who was responsible to take
initiative to organize certain educations.
Mostly
they seemed to be set up and funded by third parties (from abroad) and had to
be approved by the county and the Central Ministry.
So
there were three “owners” in the triangle who could take initiative …
In
our exploration to have an idea of the relevant size of public, private not for
profit (confessional) and private for profit health care provision, we got
quite substantial different figures regarding the source.
She
spoke about fifty public facilities in a total of three hundred.
Only
some private centres received money from the government as for example “Hope
for Women.”
Her
slightly submissive, uncertain attitude towards our inquisitory asking turned
triumphantly in a confident clinical authority when I had to beg her for the
toilet because of diarrhoea and she provided me with Flagyl to kill the
beasts.
We
visited a health centre where a team of five nurses and physician assistants
provided consultations
without the supervision of a doctor.
He
had had his education as a gynaecologist
obstetrician in
in the United States
and had worked there for many years.
He
corrected my conviction that chemotherapy was
not administered
in JFK (I
thought only planned for the gynaecology
tumours in September)
as he referred for example to chemo for Burkitt lymfoma with children.
I
was surprised
that children
oncology, which
was a high specialized
service in some University Hospitals
in Belgium, seemed to be a common practice in this hospital.
Mr.
Slewi, member of
the NCD unit and responsible for
the cancer registry, explained that
they were preparing since
2012.
They
had collected
data on a monthly basis
from six facilities since
May of this year. The most important source
of registration
was the pathologist’s diagnosis
within the JFK hospital.
They
also gathered
cancer reporting
from other centres without
pathological confirmation,
but they tried to convince the treating doctor
to refer these patients for
a pathological confirmation
in the JFK.
I
was also difficult to eliminate doubles:
patients who were seeking for different advices
in different centres.
By
the lack of a national identification
number, they asked names, birthdates, addresses and telephone numbers but as mentioned these data were not reliable.
Johnson
emphasized on
education and
awareness of
cancer issues:
“illiteracy
is the biggest problem in
this country “
At
that moment
data were collected by a standardized
registration form,
Slewi showed me,
that was filled in by a doctor or mainly by the pathologist.
He
showed us his small desk and dusty computer
donated by the WHO, where he was putting the data into an excel file, so he could make some statistic overviews.
A
special input software
from the African Cancer
Registry Organization
would soon be available but there was no link with the government
database DHIS2.
Nicholas
De Borman, head
of the Belgian software
consultancy company
Bluesquare,
who had already done
some work for the PBF unit of Vera Mussah, emphasized
that all applications and
apps developed
for low and middle intercom countries should
better be integrated
within the DHIS2 system.
During
a late lunch in a fancy African restaurant, Vera noticed me that it was forbidden to take pictures of people without
their permission.
She
didn't notice
that I was seduced by the African colours of the paintings
on the wall more than the people in the restaurant.
Not
respecting the
time schedule
because of my unsatisfiable
curiosity, we missed the appointment with
the WHO lady and - I presume the dean of the faculty of medicine had left the spot where we would have met him:
At
the Ministry, we had a last reunion to prepare the mission of August.
Embraced
by the NCD-team that did a lot of effort to make the mission happen.
Glad
being part of this dream team…
Back in the hotel I requested the receptionist
to provide me with a confirmation of my room reservation in August.
She did not succeed - due to the failure of the
Internet - and despite five reminders from my side, to make a confirmation
until just before I left the next day at twelve o'clock, although on paper,
because she could not send an email because of the internet that was being shut
down.
I did not know whether I should be angry or
have pity.
As a perfect host, Vera escorted me to the
airport or was there for another half an hour with me to taste the luxury of
the Farmington Hotel built by the Chinese.
I posed for her in the garden and at the river
and rewarded her with a lunch and a delicious glass of white wine.
Finally, she had fulfilled a Celestine promise
for me.
With thanks to :
-the NCD team for preparation and guidance of the visit
-Lonely Planet West Africa
-Lut Brugmans voor de omzetting van klank naar tekst
-Lonely Planet West Africa
-Lut Brugmans voor de omzetting van klank naar tekst